While Haliburton County won’t be one of the 26 rural communities to benefit from the first batch of internationally-trained physicians arriving via the new Practice Ready Ontario program, local recruiters have confirmed two new family doctors will start practising in the area in early 2025.
Dr. Mimi Van Der Leden is joining the Kinmount and District Health Centre (KDHC) full-time in February, while Dr. Sharysse Kayoumedjian is joining the Haliburton Family Medical Centre (HFMC) on a part-time basis in March.
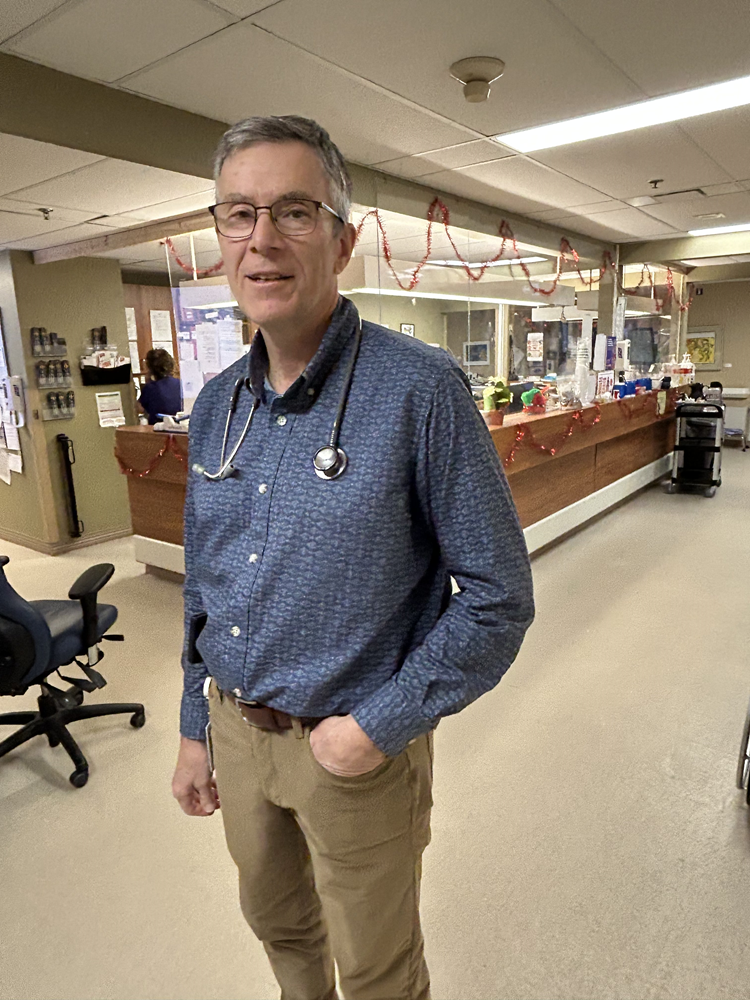
For the Kinmount centre, this is the second new addition in as many years after Dr. Lesslie Ponraja relocated to the community from the UK in February 2023. Dr. Norm Bottum, who practices at HFMC, said Kayoumedjian is the first new family physician in Haliburton for more than three years. She will be partially taking over Dr. Christina Stephenson’s practice. Stephenson retired in July 2023.
“It’s welcome news, but we could still stand to add another three or four doctors to Haliburton County,” Bottum said. “We have a long waiting list that we haven’t been able to take any patients off of for close to six years now. An easy guess would be 2,000 to 3,000 patients in Haliburton County don’t have a regular physician.”
HFMC has a roster of approximately 10,000 patients, Bottum said.
Kinmount launches new waitlist
Hannah Jensen, Ministry of Health spokesperson, said there are approximately 3,080 people voluntarily registered with Health Care Connect – the program that matches Ontarians with a family doctor – in the County and Kawartha Lakes.
Susan Forrester, a volunteer with KDHC, said the Kinmount practice should be able to shave a good chunk off that waitlist with Van Der Leden expected to take on approximately 1,500 new patients when she arrives. She said the KDHC waitlist has over 1,000 people.
Area residents who do not have a family doctor are asked to join a new waitlist by applying at forms.gle/ tnYDLfSVDnwMXSby9.
It’ll be a true north homecoming for Van Der Leden – she grew up in eastern Ontario and graduated from Montreal’s McGill University before obtaining her MD PhD from the University of Illinois. She was most recently practicing in the Chicago area.
“This is big news for Kinmount and for the wider community – family medicine is hard to access in rural Ontario. We’re competing with other communities not only here, but across the country, and across the world,” Stevenson said. “Dr. Van Der Leden is excited about relocating here – she’s visited multiple times this year and has spoken about enjoying nature, the feel of the community. We’re lucky to have her.”
Practice Ready Ontario
There was a period in the fall when Forrester and the rest of the KDHC team thought they might have been getting two new doctors.
Kinmount was in the running for another U.S. based physician until recently. That doctor was approved in the first batch of overseas physicians graduated through the provincial Practice Ready Ontario program, though chose to work in another community.
The file removes requirements to complete years-long re-education programs, introducing 12-week assessments applicants must pass to prove they have the skills needed to practise here. Once approved, the doctors are required to complete a three-year return of service as a family doctor in a rural or northern community.
The province said it plans to bring 100 new doctors to Ontario in 2025.
Haliburton, Kawartha Lakes, Brock MPP Laurie Scott said she’s hearing Canada is an increasingly attractive destination for overseas docs.
“We know we have a shortage of doctors in Ontario, so we’re trying to make it as easy as possible for qualified physicians to come here. Our recruitment people are saying they’re getting positive responses. We still have some vacancies to fill, so I hope our teams and communities continue to apply,” Scott said.
Wendy Welch, Haliburton County’s doctor recruitment coordinator, said she did not apply. “Our physician team investigated Practice Ready Ontario but, unfortunately, do not have the capacity to participate.”
Bottum said he’ll reserve judgement on the program. He says any attempts to bring additional qualified doctors to Ontario is a positive thing, though he believes the province should prioritize training more physicians here.
“We’ve been so poor in Ontario graduating medical students. We’ve known, literally, for decades that we’re not graduating enough,” Bottum said. “What the government should be doing, instead of focusing on overseas, is getting to the point where we have a surplus of doctors here in Ontario, so that we can help other parts of the country.”
The province announced last fall it would be investing $88 million over three years to expand Learn and Stay grants for 1,360 eligible Canadian undergraduates who commit to practice family medicine with a full roster of patients once they graduate.
It’s estimated the investment will connect an additional 1.36 million people to primary care by 2028.
Bottum said it’s a good start, but more is needed. He believes a lack of family doctors in the area is driving people to the busy Haliburton Highlands Health Services emergency room, estimating 75 to 80 per cent of patients who require acute care don’t have one.
“This failure goes back decades – we’ve ended up in this terrible situation where almost every government for the past 30-plus years has ignored health care,” Bottum said.